Iron deficiency anemia remains one of the most prevalent nutritional disorders worldwide, affecting individuals across all age groups. The condition arises when the body lacks sufficient iron to produce hemoglobin, the protein in red blood cells responsible for oxygen transport. Without adequate iron, the body struggles to generate healthy red blood cells, leading to fatigue, weakness, and a host of other symptoms. Addressing this deficiency requires a well-structured iron supplementation plan tailored to individual needs.
The first step in any iron supplementation regimen is accurate diagnosis. Physicians typically rely on blood tests to measure hemoglobin, serum ferritin, and other markers of iron status. It’s not uncommon for individuals to mistake general fatigue for iron deficiency without proper testing, which can lead to unnecessary or ineffective treatment. Once diagnosed, the focus shifts to replenishing iron stores through dietary changes, oral supplements, or in severe cases, intravenous therapy.
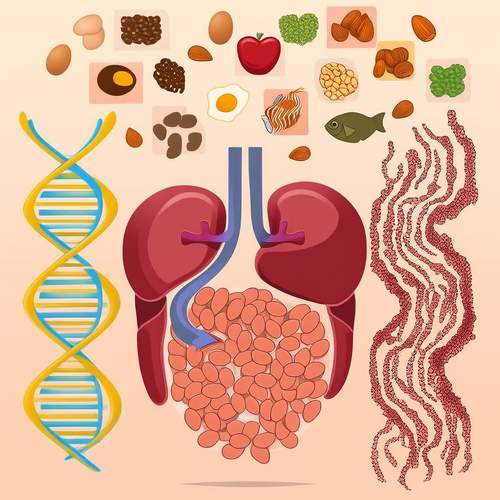
Dietary adjustments play a pivotal role in managing mild iron deficiency. Iron exists in two forms in food: heme iron, found in animal products like red meat and seafood, and non-heme iron, present in plant-based sources such as lentils and spinach. Heme iron is more readily absorbed by the body, making it a preferred option for those with deficiencies. However, vegetarians and vegans can still meet their iron needs by combining non-heme iron with vitamin C-rich foods, which enhance absorption. Avoiding inhibitors like coffee, tea, and calcium-rich foods during iron-rich meals is equally important.
For those unable to meet their iron requirements through diet alone, oral iron supplements are often recommended. Ferrous sulfate, ferrous gluconate, and ferrous fumarate are among the most commonly prescribed forms. While effective, these supplements can cause gastrointestinal side effects such as constipation or nausea. To mitigate these issues, healthcare providers may suggest starting with a lower dose and gradually increasing it, or taking the supplement with food—though this may slightly reduce absorption. Consistency is key, as iron levels take time to rebuild.
In cases of severe deficiency or malabsorption disorders, intravenous iron therapy may be necessary. This method delivers iron directly into the bloodstream, bypassing the digestive system altogether. It’s particularly beneficial for individuals with conditions like inflammatory bowel disease or those who’ve undergone bariatric surgery. While IV iron can rapidly restore iron stores, it requires medical supervision due to potential allergic reactions or other complications. The choice between oral and IV iron depends on the severity of the deficiency, underlying health conditions, and patient tolerance.
Monitoring progress is an often-overlooked yet critical component of iron supplementation. Follow-up blood tests help determine whether the chosen method is effective or if adjustments are needed. Some individuals may see improvements in symptoms within weeks, but it can take several months for iron stores to fully replenish. Patience and adherence to the prescribed plan are essential for long-term success.
Beyond supplementation, addressing the root cause of iron deficiency is vital. For many, it stems from chronic blood loss—commonly due to heavy menstrual periods or gastrointestinal bleeding. In such cases, treating the underlying issue prevents recurrence. Pregnant women, growing children, and athletes are also at higher risk and may require ongoing iron support. A holistic approach that combines supplementation with lifestyle and medical interventions offers the best chance for sustained recovery.
Public awareness about iron deficiency remains surprisingly low, given its widespread impact. Many people dismiss symptoms like persistent tiredness or pale skin as mere stress or lack of sleep. Education campaigns highlighting the importance of iron in overall health could lead to earlier detection and treatment. Simple measures, such as routine screening for high-risk groups, could significantly reduce the burden of this preventable condition.
While iron supplementation is generally safe, excessive intake can lead to toxicity, particularly in individuals without a deficiency. Symptoms of iron overload include nausea, vomiting, and even organ damage in severe cases. This underscores the importance of professional guidance before starting any iron regimen. Self-diagnosis and unsupervised supplementation can do more harm than good.
The journey from iron deficiency to restored health is rarely linear. It requires a combination of medical insight, patient commitment, and sometimes, trial and error to find the most effective approach. With the right strategy, however, iron deficiency anemia is not just manageable—it’s reversible. The key lies in personalized care, ongoing monitoring, and a clear understanding of how iron functions within the body.

By /May 21, 2025
By /May 21, 2025

By /May 21, 2025
By /May 21, 2025
By /May 21, 2025
By /May 21, 2025
By /May 21, 2025

By /May 21, 2025

By /May 21, 2025

By /May 21, 2025

By /May 21, 2025

By /May 21, 2025
By /May 21, 2025

By /May 21, 2025

By /May 21, 2025

By /May 21, 2025

By /May 21, 2025

By /May 21, 2025

By /May 21, 2025

By /May 21, 2025