Cholesterol metabolism has long been a focal point in nutritional science, particularly as it relates to cardiovascular health. The way our bodies process dietary cholesterol is far more complex than the outdated "good vs. bad" dichotomy suggests. Emerging research continues to reveal how individual genetic factors, gut microbiota composition, and specific food matrices influence cholesterol absorption and endogenous production. This nuanced understanding is reshaping dietary recommendations beyond simple cholesterol avoidance.
The liver serves as the metabolic hub for cholesterol regulation, producing about 80% of the body's cholesterol while carefully balancing intestinal absorption of dietary sources. What makes this system remarkable is its feedback mechanisms—when dietary intake increases, hepatic synthesis typically decreases. However, this regulatory system functions differently across individuals due to polymorphisms in genes like APOE and NPC1L1. These genetic variations explain why some people can consume cholesterol-rich foods with minimal impact on serum levels while others show pronounced responses.
Dietary fats demonstrate surprising paradoxes in cholesterol metabolism. While saturated fats were traditionally vilified for raising LDL cholesterol, we now recognize that specific saturated fatty acids have divergent effects. For instance, stearic acid (abundant in dark chocolate) appears neutral, while lauric acid (found in coconut oil) may elevate both LDL and HDL. The food matrix matters tremendously—eggs consumed with fiber-rich vegetables affect cholesterol metabolism differently than when eaten with processed meats. This explains why population studies often contradict controlled feeding trials.
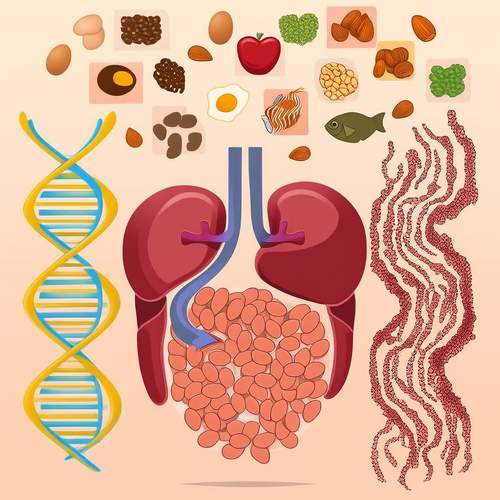
The gut microbiome has emerged as a critical player in cholesterol homeostasis. Certain bacterial species like Bacteroides dorei can metabolize cholesterol into coprostanol, a non-absorbable compound excreted in feces. Regular consumption of fermented foods rich in probiotics may enhance this beneficial conversion. Simultaneously, prebiotic fibers act as substrates for bacteria that produce short-chain fatty acids, which downregulate hepatic cholesterol synthesis through epigenetic mechanisms. This gut-liver axis represents a promising target for dietary interventions.
Plant sterols and stanols continue to demonstrate clinically meaningful LDL reductions of 8-10% at doses of 2g/day, yet their mechanism is often misunderstood. Rather than simply blocking cholesterol absorption, these phytochemicals accelerate the liver's LDL receptor activity through complex signaling pathways. The practical challenge lies in incorporating therapeutic doses through whole foods rather than relying solely on fortified products. Sesame seeds, pistachios, and cold-pressed oils provide natural sources that synergize with other cardioprotective nutrients.
Time-restricted feeding patterns are revealing fascinating connections between cholesterol metabolism and circadian biology. Bile acid synthesis follows a diurnal rhythm, peaking during active hours when food is typically consumed. Disrupted eating patterns may impair cholesterol clearance as bile acid production becomes desynchronized. This explains why shift workers often exhibit unfavorable lipid profiles despite similar macronutrient intakes to day workers. Aligning meals with natural light cycles appears to optimize cholesterol turnover.
The interplay between dietary cholesterol and vascular inflammation warrants careful consideration. Oxidized LDL particles—not cholesterol itself—drive atherosclerotic processes. Antioxidant-rich foods like berries, extra virgin olive oil, and green tea may mitigate this oxidation while paradoxically allowing higher dietary cholesterol tolerance. This protective effect underscores why Mediterranean diets, often containing moderate cholesterol from fish and eggs, consistently outperform low-fat diets in cardiovascular outcomes.
Emerging evidence challenges conventional wisdom about dietary cholesterol and aging. Elderly individuals frequently show reduced cholesterol absorption efficiency and altered hepatic synthesis. Some geriatric studies suggest that moderately cholesterol-rich diets may support neurocognitive function and hormone production without adversely affecting cardiovascular risk markers. This highlights the importance of life-stage-specific nutritional guidance rather than universal cholesterol restrictions.
Practical dietary strategies for optimizing cholesterol metabolism should emphasize food synergy over isolated nutrients. Combining soluble fiber with cholesterol-containing foods, pairing healthy fats with polyphenol-rich plants, and timing meals to align with natural rhythms appears more effective than simplistic cholesterol avoidance. As research evolves, personalized approaches considering genetics, microbiome composition, and metabolic phenotype will likely replace one-size-fits-all recommendations.

By /May 21, 2025
By /May 21, 2025

By /May 21, 2025
By /May 21, 2025
By /May 21, 2025
By /May 21, 2025
By /May 21, 2025

By /May 21, 2025

By /May 21, 2025

By /May 21, 2025

By /May 21, 2025

By /May 21, 2025
By /May 21, 2025

By /May 21, 2025

By /May 21, 2025

By /May 21, 2025

By /May 21, 2025

By /May 21, 2025

By /May 21, 2025

By /May 21, 2025